A phlebotomist is seen holding a unit of blood after a blood donor had blood taken from him at the Ottawa Blood Services clinic.
Photograph by: Chris Roussakis / Postmedia , Postmedia News
Part 1
When doctors at a New Jersey hospital pioneered a “bloodless” surgery program for patients who refused blood transfusions on religious grounds, they discovered something totally unexpected: Jehovah’s Witnesses, who would choose death over a transfusion, recovered just as well as transfused patients — and in many cases, even better.
They suffered fewer post-surgery complications, spent less time on mechanical breathing machines and had shorter stays in intensive care.
Recently, doctors from the Cleveland Clinic in Ohio reported that Jehovah’s Witnesses who refused blood transfusions while undergoing cardiac surgery were significantly less likely to need another operation for bleeding compared with non-Witnesses who were transfused. They were also less likely to suffer a post-op heart attack or kidney failure.
Are the Jehovah’s Witnesses onto something?
In cases of massive “bleed outs” from trauma or hemorrhage, or for patients with leukemia or other cancers, blood transfusions can be lifesaving.
At the same time, experts say there is remarkably little evidence to show which patients — short of those suddenly losing large amounts of blood — actually benefit from blood transfusions.
In fact, a growing body of research links transfusions with an increased risk of post-surgery infections, cardiac arrest, heart attack, stroke, kidney failure, lung injury, multi-organ failure and death.
Transfused patients spend more time in hospital than those who don’t get
blood; they spend more time in intensive care units connected to ventilators;
and have a higher risk of acute respiratory distress, where the lungs become
saturated with fluid, preventing enough oxygen from getting to the lungs and
into the blood.
Studies suggest that up to half of all red-blood-cell transfusions may be unnecessary. Needless transfusions not only waste blood, they expose patients to risks — including potentially life-threatening human errors that are occurring at every step in the transfusion chain.
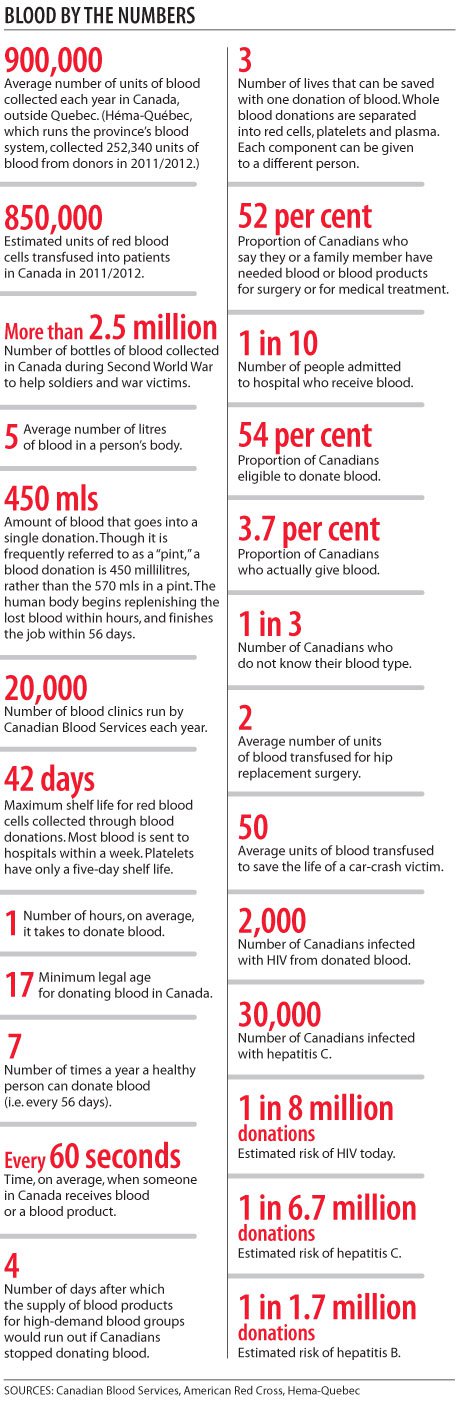
Three decades after Canada’s catastrophic tainted-blood tragedy left 2,000 people infected with HIV and another 30,000 with hepatitis C, the greatest threat to patients today isn’t the risk of contracting an infectious disease from blood, experts now say.
It’s getting blood they don’t need.
—-
From ancient times to the late 19th century, sickness was treated by blood loss: using lances or leeches to bleed the body of suspected diseases that caused “bad” blood.
Today, we call blood the “gift of life.” The belief that blood is almost a magical cure is still held by many.
“In the minds of many people, blood is life, and giving people blood must help life,” says Dr. Jacques Lacroix, a professor of pediatrics at the University of Montreal and a national and international pioneer in pediatric critical care and research.
“But it does not work like that.”
.jpg)
A phlebotomist is seen holding a unit of blood at the Ottawa Blood Services clinic. Chris Roussakis/Postmedia
In fact, transfusions have been identified by the American Medical Association as among the top five overused procedures in medicine.
In Canada, about 850,000 units of red blood cells, and 102,000 doses of platelets, were transfused into patients outside Quebec in 2011-2012, according to estimates compiled by the Canadian Blood Services for Postmedia News. (Hema-Quebec, which runs the province’s blood system, collected 252,340 units of blood from donors in 2011-2012; more than 526,000 blood products were shipped to hospitals.)
Canadian researchers have led the world in showing that patients benefit from more restrictive blood use. But, there is no single, unified national system to determine how much of the blood distributed by the Canadian Blood Services is actually transfused, who gets it and whether it’s being given for the right reasons.
Studies suggest that, even when patients have the same underlying condition, the same surgery and the same blood loss, transfusion rates vary widely from hospital to hospital for the same operation.
For example, a review of more than 8,000 patients who underwent cardiac surgery in British Columbia between 2008 and 2010 found that the proportion of patients who received red-blood-cell transfusions ranged from 35 to 66 per cent.
A province-wide audit of Ontario hospitals published in May concluded that nearly one in three transfusions of frozen plasma — the liquid portion of blood that contains clotting factors to help control bleeding during surgery — was unnecessary.
In Calgary, knee replacement patients are being transfused at rates ranging from two per cent of patients to 25 per cent, depending on the surgeon.
Many transfusions don’t meet even minimum published guidelines, experts say. Many patients receive not one, but multiple units of blood, increasing their risk of fluid overload, where the extra blood overwhelms the heart’s ability to pump it through the body. Transfusion-related circulatory overload is one of the leading causes of transfusion-related death.
In some areas of medicine, including cardiac surgery, no clear consensus exists on when patients should be transfused.
“What we are sure of, however, is that there is a huge variation in transfusion rates across Canada for cardiac surgery patients of the same risk profile, and this is very difficult to explain,” says Dr. Fraser Rubens, a cardiac surgeon at the University of Ottawa Heart Institute.
—-
As concern mounts over the dangers of unnecessary transfusions, hospitals have begun using strategies to reduce the use of blood.
For example:
-Blood draining out from under surgical wounds is being siphoned off, re-processed and then re-infused back into the patient;
-Surgeons are using drugs to prevent bleeding and improve blood clotting;
-Surgeons are operating through laparoscopes and other minimally invasive tools to reduce bleeding from large surgical wounds;
-Patients are being screened and treated for anemia with supplements or drugs that boost the bone marrow to produce red blood cells before they get into the operating room.
The variability in transfusion rates is slowly falling. But doctors have been slow to adapt. “The biggest challenge is trying to change the behaviour of physicians,” says Dr. Alan Tinmouth, a hematologist and scientist at the Ottawa Hospital Research Institute. “People are being transfused at hemoglobin levels higher than they need to be.”
Many doctors remain unconvinced of the potential dangers of transfusions. None of the studies suggesting increased risks of harm prove cause-and-effect, just an association, they point out. What’s more, patients who are transfused tend to be sicker to begin with, so it’s no surprise that they don’t recover as well as non-transfused patients, they argue.
But Dr. Paul Marik says numerous studies have shown that the more blood given, the worse the outcome.
In a widely cited study published in 2008, Marik analyzed 45 studies involving nearly 300,000 patients. In 42 of those studies, the risks of red-blood-cell transfusions outweighed the benefits. Transfused patients were twice as likely to develop infections, multi-organ failure and acute respiratory distress than the non-transfused.
Critics of his conclusions say many of the older studies were done before white cells were filtered out of whole-blood donations. White cells in the “host” body help fight disease and infection. But when they’re put into someone else, they can suppress the immune system.
More recent studies have shown that transfusion-related reactions have fallen since blood suppliers began washing white blood cells from blood. However, Dr. Aryeh Shander, clinical professor of anesthesiology, medicine and surgery at Mount Sinai School of Medicine in New York, says that while there has been an unquestionable reduction in fever rates, “the rest is debated.”
Shander helped create the bloodless medicine and surgery program at Englewood Hospital and Medical Center in Englewood, New Jersey. He says that “old habits die hard” and that too many doctors believe “something bad will happen” if patients don’t have a certain volume of blood in their system.
—-
The biggest driver of red-blood-cell transfusions is hemoglobin, the protein in red blood cells that ferries oxygen from the lungs to tissues and cells throughout the body. Too little hemoglobin, and the person becomes anemic.
Red blood cells are frequently transfused during cardiac surgery, prostate surgery, joint replacements and in patients bleeding from their intestinal tracts.
But, once removed from the body, red cells undergo changes in their shape and function. Their membranes deteriorate; some cells burst, releasing free hemoglobin, which mops up nitric oxide, the chemical that helps blood vessels relax. There are now growing concerns that “older” red cells stored for longer than a few weeks lose some of their ability to transport oxygen — the very reason they’re transfused. In Canada, red cells are stored for up to 42 days.
When he was in medical school, Ottawa critical care specialist Dr. Paul Hebert, whose research has transformed transfusion practices worldwide, was taught that seriously ill patients need a high level of hemoglobin to keep diseased or damaged tissues alive. So ingrained was this belief that anesthesiologists and surgeons routinely began transfusing surgery patients if their hemoglobin dipped below a certain number (100 grams per litre of blood.)
In a landmark paper published in the New England Journal of Medicine, Hebert and his team found that patients who were only mildly below that hemoglobin cutoff, but who were treated aggressively with transfused blood nonetheless, were more likely to die, and had higher rates of organ failure, than patients whose doctors held back until their hemoglobin fell to lower levels.
“We found that, if you give less blood, you do better,” Hebert said. “We think that’s because many of the patients didn’t need it in the first place.”
In a study published in January 2013, Hebert and co-authors reviewed 19 trials involving more than 6,000 patients that compared higher versus lower hemoglobin thresholds in red-blood-cell transfusions. They found that patients could be transfused at hemoglobin levels of 70 or 80 grams per litre of blood without putting them at any increased risk for major complications such as pneumonia, stroke, infection, or death.
If doctors were to use the lower thresholds, “I think you can reduce blood use in many settings by at least half,” said lead author Dr. Jeffrey Carson, chief of the division of general internal medicine at Rutgers Robert Wood Johnson Medical School in New Brunswick, New Jersey.
A recent review of blood transfusions at three Ontario hospitals found that the pre-transfusion hemoglobin levels were higher than the recommended thresholds for many patients.
Some transfusion rates have been falling since the province established a network of blood transfusion co-ordinators in 25 hospitals. A major thrust of the program is to treat patients with anemia — low hemoglobin — before surgery “so that we avoid having to transfuse them when they bleed,” said Dr. John Freedman, medical director of the program and professor emeritus at the University of Toronto.
British Columbia created the first transfusion registry in Canada in 1999; it remains one of the largest in North America. The database tracks every unit of blood that gets transfused into someone in B.C or the Yukon.
Within the year, The Ottawa Hospital hopes to have a computerized system in place to capture where blood is going, which patients are being transfused and their hemoglobin levels at transfusion.
While Jehovah’s Witnesses have taught doctors that the body can compensate for extraordinarily low levels of hemoglobin, levels that are too low mean the cells and tissues in the brain and other vital organs become starved of oxygen.
Hebert has watched Jehovah’s Witnesses die for refusing to be transfused, an experience that leaves the medical team feeling helpless. “But you can’t force your values on someone else,” he says.
Hebert says more research and education is needed to help doctors decide how long they can safely wait before ordering blood, how much blood they should give and when to hold off giving any blood at all.
“The problem is that we don’t have the data,” Hebert said. “In many cases, we
just don’t know.”
.jpg)
A phlebotomist is seen holding a unit of blood after a blood donor had blood taken from him at the Ottawa Blood Services clinic.
Photograph by: Chris Roussakis / Postmedia, Postmedia News
Calgary Herald Headline News





.jpg)











